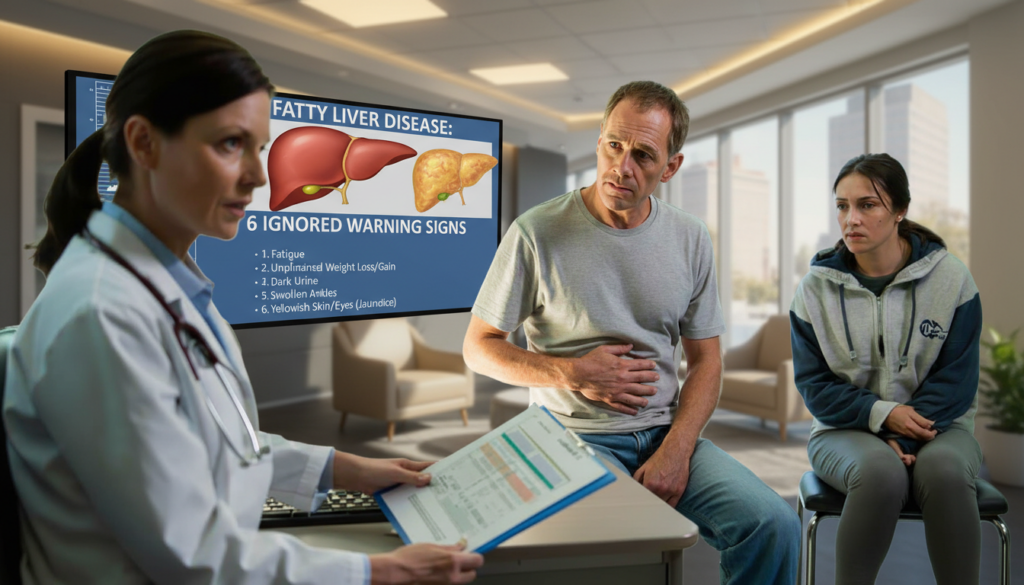
The waiting room was full, but it was quiet in that tense way where people act like they’re scrolling through their phones but can hear every word through the door. A man in his forties walked out of the hepatologist’s office looking shocked and staring at a brochure as if it were in a different language. A woman in leggings and a work hoodie came out a few minutes later, her eyes glazed over, saying to herself, “But I don’t even drink.”
We’ve all been there: when a doctor says something that doesn’t fit with what we tell ourselves about our health.
Fatty liver disease is the main reason for this mismatch. It doesn’t always hurt. It doesn’t yell. It just settles in quietly while life goes on: emails, kids, late dinners, a glass of wine, or maybe two.
One thing the hepatologist I met that day said stuck with me.
People don’t just miss the signs; they often deny them.
“I Feel Mostly Fine”: The Silent Progression No One Wants to Hear About
The first thing this expert said was so simple that it was almost funny: most people with fatty liver disease say they “feel fine.” Then they say, “I’m just a little tired, but that’s life, right?” She is most worried about that vague, dragging tiredness because people often think it’s just stress, getting older, or not getting enough sleep.
She talked about patients who get through their days on coffee and willpower, believing that being busy is just part of the deal. The liver is working too hard because it has too much fat. But from the outside, it looks like normal life in the 21st century.
She told me about a 38-year-old delivery driver who had two kids and came in for regular blood tests that he needed for work. Increased liver enzymes. Ultrasound. Diagnosis: non-alcoholic fatty liver disease, which is already getting close to inflammation.
He didn’t have any severe pain or symptoms. He joked that his “dad tank” was always tired, had some brain fog, and a stubborn belly. At first, he laughed when the doctor talked about his liver, but he stopped when she showed him the pictures.
Women in their thirties and forties do the same thing: they blame their lack of energy on kids, night shifts, or hormones. The story sounds different, but the lab results look very much the same.
The truth is that our culture makes it normal to feel tired, bloated, and a little sick.
The hepatologist said that fatty liver disease slowly gets worse as fat gets into liver cells. At first, the organ is still able to handle it. It has a strong filter that can heal itself more than most organs can. But too much fat causes inflammation and then scarring over time. That’s when it gets harder to change things back.
The “mild” signs—tiredness, heavy digestion after meals, pressure under the right rib, and unexplained weight gain around the waist—are like a fire alarm that isn’t very loud. Not a siren yet, but definitely not quiet.
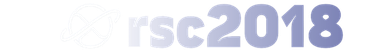
The 6 Signs That People Say Are “Nothing Serious”
When we talked about the details, the doctor brought up the same six red flags that people keep ignoring. First, you feel tired all the time, even when you’re not working. Second, you might feel heavy or a little pressure on the right side of your upper abdomen, especially after eating. Third, unexplained weight gain in the stomach, even if the scale doesn’t move much.
The fourth sign shocked me: nausea that comes and goes or a slight loss of appetite on some days, followed by strong cravings on others. Fifth, blood tests that show abnormal liver enzymes that people ignore because they “feel fine.” And sixth: a dull brain fog that makes it hard to focus and forget simple things more often than usual.
She told me about a teacher who had four of those signs for a long time. She thought her stomach pain was just gas, her brain fog was “end-of-term burnout,” and her lab results were “a bit off, but nothing dramatic,” as her doctor had said before.
When she finally saw the hepatologist, the ultrasound showed that her liver was inflamed. Early-stage steatohepatitis is when fatty liver goes from being a quiet guest to a destructive one. What did the teacher do? “I thought only alcoholics got cirrhosis.”
That sentence is still heard in a lot of consultation rooms. Millions of people who don’t drink much or only on weekends and feel “reasonable” about it now have non-alcoholic fatty liver disease.
It’s very easy to see why these six signs make sense. The liver is where metabolism happens: fats, sugars, toxins, and hormones. It can’t filter, control, or store energy as well when it has too much fat. When you’re tired, your body is telling you that the system is in emergency mode.
Abdominal pressure happens when the liver swells a little or when the tissues around it change. Brain fog is often a sign of metabolic problems that affect both the brain and the liver. The sneaky part is that each sign by itself looks boring. When you put them all together, they make things look a lot worse.
This is why the hepatologist keeps saying the same thing over and over: “One sign could be a coincidence.” A check-up is needed for two or three of them.
What a Hepatologist Wants You to Do Right Away If You Have Any Doubts
When I asked her what she wanted people to do earlier, her answer was surprisingly sensible. Not a miracle cleanse. Not a strange supplement. Just a simple, down-to-earth sequence.
First, don’t romanticize your tiredness as productivity; just listen to it. Second, keep a record of your symptoms for two weeks, including how tired you are, how well you digest food, how uncomfortable you feel, how hungry you are, and how you feel. Third, schedule a blood test that includes liver enzymes and talk to a doctor about your notes.
“People come late because they wait for pain, and fatty liver doesn’t always follow the pain rule,” she said.
She said she gets why people deny it. No one wants to hear that their way of life is hurting an organ they can’t even feel most of the time. A lot of her patients are ashamed and think they “failed” at health, especially when weight or alcohol come up.
She tries to get rid of that shame right away. Genetics, sleep, stress, ultra-processed foods, and sedentary jobs are all strongly linked to fatty liver. These things don’t make you a bad person; they’re just things that happen to people in 2026. The problem isn’t the condition itself. The mistake is thinking it’s not worth checking because “everyone is tired” or “my belly has always been like that.”
The hepatologist said quietly, “People tell me, ‘I don’t want to know; it will stress me out.'” “But the stress of not knowing while the disease gets worse is much worse than the stress of catching it early, when we still have a lot of power to stop it.”
- Pay attention to patterns instead of just one day of feeling tired or sick.
- When you get your blood tested, ask your doctor directly about your liver.
- Even if you feel fine, don’t downplay abnormal liver enzymes.
- Don’t just think of your waistline as a fashion issue; think of it as a health issue.
- Even if you think your drinking is “moderate,” be honest about it.
A Quiet Organ, Loud Results
The ironic thing about fatty liver disease is that the organ that is the main character never gets a voice. The heart can race, the lungs can hurt, and the stomach can cramp. The liver doesn’t say much until the damage is really bad. That’s why these six small signs are so important; they’re like whispers through a closed door.
Once fibrosis starts, the path can lead to cirrhosis, liver cancer, or transplant lists. That’s the part that no one wants to think about, but it’s what makes some people who used to deny it make radical, life-saving changes. And if you start those changes early enough, they can really change the story.
 Heavy snow confirmed to intensify overnight as meteorologists warn of whiteout risks Update
Heavy snow confirmed to intensify overnight as meteorologists warn of whiteout risks Update
| Key point | Detail | Value for the reader |
|---|---|---|
| Recognize the 6 subtle signs | Fatigue, right-side heaviness, belly weight, nausea/cravings, abnormal labs, brain fog | Helps you spot potential fatty liver disease before serious damage |
| Act on doubt, not on pain | Track symptoms, request liver tests, discuss results clearly with a doctor | Gives you a chance to reverse or slow progression while it’s still possible |
| Drop the denial narrative | Understand this isn’t just an “alcoholic’s disease” or a “lazy” problem | Reduces shame and motivates realistic, compassionate lifestyle changes |
Frequently Asked Questions:
Question 1: Can fatty liver disease really be reversed after it is found?
Question 2: Do I have to drink alcohol to get fatty liver disease?
Question 3: What tests should I ask for if I think I have fatty liver disease?
Question 4: Is it possible for skinny people to have fatty liver disease?
Question 5: How long does it usually take for changes in lifestyle to make the liver better?
 Meteorologists warn early February atmospheric signals point to a dangerous Arctic anomaly Update
Meteorologists warn early February atmospheric signals point to a dangerous Arctic anomaly Update